When Nigerians dream of moving to the UK for better opportunities, they rarely picture sleepless nights, high-risk patients, and barely scraping by. Yet, for thousands of Nigerians who have made the move, care and support work is the stepping stone to a better life — or at least survival.
We spoke to four Nigerians to understand what it means to build a life in the UK’s care sector and how their income compares to what they left behind in Nigeria.
“The hardest part is when they shout at me, but I’ve developed a thick skin.” —Ehi, 32, £2,000/ Month.

When I moved to the UK in 2023, I left behind a stable life as a dentist in Lagos. Back home, my white coat and years of training earned me respect. Now, as a support worker in Nottingham, I spend my days assisting people with disabilities and mental health challenges. While it’s meaningful, it doesn’t demand the same level of critical thinking or problem-solving I once thrived on, and I miss that.
I had to find a way to survive financially while pursuing my long-term goal: passing the UK dentist licensing exams, which cost thousands of pounds. Support work was the obvious short-term choice.
It wasn’t always easy. When I first arrived as a student, strict work-hour limits meant I barely scraped by. At the time, I even worked in a warehouse, pushing through shifts that paid £500 monthly — a striking contrast to my ₦278k base salary (plus ₦300k–₦500k in commissions) as a Lagos dentist.
But now that I’ve completed my master’s in public health, I work full-time in support, earning £2,000 per month. My wife, who came as my dependent, also works in a care home, bringing in £1,500 monthly. Together, we manage rent, bills, and savings, painfully aware that every penny counts toward my next career move.
My ultimate goal is to secure sponsorship, pass my licensing exams, and return to practising dentistry, where salaries range from £50k—£100k per year. With sponsorship, I’d get a three-year work permit, which can be renewed. After working for five years in total, I can apply for Indefinite Leave to Remain (ILR), essentially permanent residency. If we have a child along the way, that could also open a pathway to staying. Still, British citizenship isn’t automatic—the child would be considered British property, meaning the government allows parents to stay to care for them.
For now, I’m relying on support work as my backup plan to secure sponsorship, remain in the UK legally, and eventually transition into my profession.
In the meantime, I put in 45-hour weeks, mostly night shifts, balancing exhaustion with hoping for something better. Support work isn’t physically draining, but dealing with patients struggling with addiction, mental health issues, or aggressive behaviour takes a mental toll.
The hardest part is when they shout at me, but I’ve developed thick skin. We use deescalation techniques — calm talking, removing dangerous objects, keeping a safe distance. Most times, they calm down and even apologise.
But despite everything, the UK is still an adjustment.
I miss the hustle and bustle of Lagos. The UK is boring. Everyone just minds their business.
For now, though, minding my business means securing my future. This support work is my backup plan. I’m laying low, putting in the hours, and waiting for the moment I can transition back to dentistry.
“An elderly man with dementia mistook me for his wife at a care home.” — Ikram, 25, £2,000/ Month.

I moved from Nigeria in September 2022 to pursue a master’s degree in digital marketing. Like many Nigerian students who needed a job to support themselves, care work seemed like the most viable option.
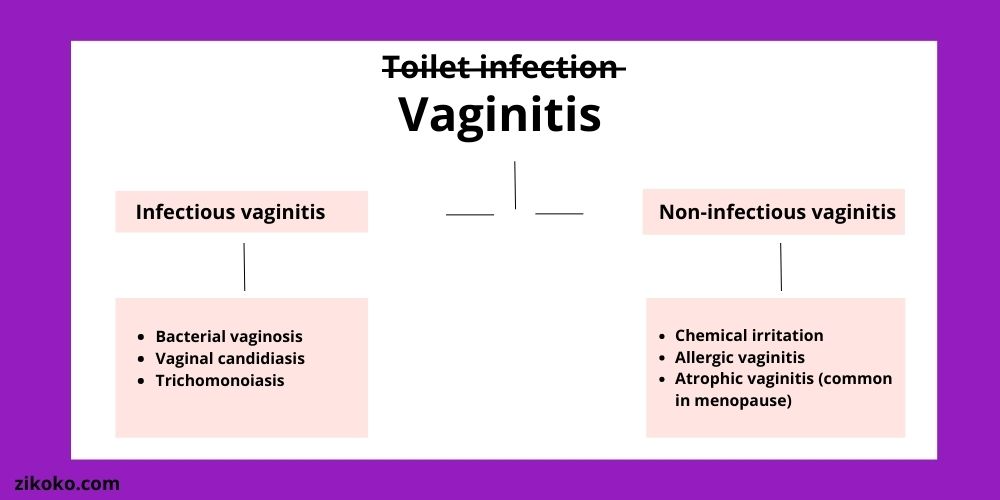
I worked for an agency that placed me in various care homes and support settings. The work was often mentally challenging. I encountered residents with a range of mental health conditions, some of whom could become aggressive or self-harm. We were trained in de-escalation techniques and restraint, but it was still tough.
There were days I had to cycle through pouring rain at 6 a.m., racing against time to make it to a support work shift because I couldn’t afford the £7 train fare while waiting for the previous week’s pay.
Then there were the lighter moments — like the elderly man with dementia who mistook me for his wife at a care home. He locked his hands in mine, brought them to his lips, kissed them, and spoke to me as if I were her. Then he said, “They have me locked up here, but as long as you’re with me, Caroline, I’ll be good.”
As a support worker, I earned £11.50 per hour, raking in around £500/ week. However, the shifts weren’t always constant, and I sometimes had to rely on my mum in Nigeria for financial support. I left care work after a dispute over my timesheet with a resident’s family member.
I got my first proper job in the UK as a marketing executive in November 2023, but my role was made redundant in January. Subsequently, I did freelance work for friends while searching for a permanent position. I finally landed a job as a digital marketing manager at the University of Wolverhampton in June 2024, which pays me £28,000 a year.
“It took five years to secure a UK Support Work Visa.” — Akinyemi, 27, £2,500/ Month.

I loved caring for my patients at my job as a healthcare assistant in a Nigerian private hospital. But the pay was barely enough to survive. I earned ₦150k per month, which covered my basic needs but left no room for savings or a future. I wanted more — better career growth, stability, and financial security.
In 2023, I moved to the UK on a work visa as a support worker after years of searching.
I studied Public Health in Nigeria, so working in healthcare felt like a natural fit. Now, I earn between £2,000–£2,500 per month, depending on my shifts. That said, I primarily work 30-40 hours a week.
While my financial situation has improved, it’s not an overwhelming surplus, mainly because the UK’s cost of living is much higher than when I lived in Nigeria. But for me, it’s more about financial stability and growth opportunities rather than just getting by. I can now save, support my family back home, and plan for the future, making a significant difference for me.
But the job itself is tough. I assist residents in care homes with personal care, meals, and daily activities. Some have severe mental health conditions or physical disabilities, and the work can be physically and emotionally draining. But there are rewarding moments — like knowing I’ve made someone’s day a little easier.
Adjusting to life in the UK wasn’t easy. Beyond the job, I had to get used to direct communication, strict workplace protocols, and even small cultural shocks — like how seriously the British take queues. But over time, I’ve learned to navigate the system and balance my work with my personal life.
I started looking for sponsorship jobs in 2018 and finally secured one in 2023. Many people rush the process and pay agents ridiculous sums, only to arrive and find no job waiting for them. But I handled everything myself — just Google, apply directly on company websites, and be patient. It took years, but in the end, it was worth it.
I have better financial stability, career prospects, and exposure to a well-structured healthcare system.
In the long term, I plan to advance in healthcare, possibly through further training or specialisation. Whether I continue progressing in the UK or explore opportunities elsewhere, my goal remains to build a fulfilling and sustainable career in healthcare.
“I lost my first support work because they snitched on me.” — Ayodele, 25, £1400/ Month.

I lost my first support work because a white woman snitched on me. She said I was sleeping on the job — which, to be fair, I was. But I got another one with the same pay, so I moved on.
Now, I work as a support worker in the UK, putting in 30–32 hours a week. It’s not physically demanding, so I manage to fit in other things — my art, partying, and hanging out with friends. But financially? It’s a constant battle. After taxes, I take home around £1,400. From that, £500 goes straight to debt settlement; some money I loaned to help me settle in the UK still needs to be paid off, leaving me with £900. Then rent takes £650, which leaves just £250 for everything else: food, transport, basic survival.
Before I finished my master’s in September 2024, I was earning £1,800. Then the tax season hit, and the tax management department for the UK government, HMRC (Her Majesty’s Revenue and Customs), started taking out £400+. I have to pay income tax for every hour I spend working, and my employer deducts it directly from my paycheck. The more you work, the more they tax you, so even picking up extra shifts doesn’t always help.
In Nigeria, I was raking in around ₦200,000/month between drawing, painting, and making portraits. However, after university, I struggled to find a good job with my biochemistry degree, so I took the next step: a one-year master’s in Public Health at the University of Birmingham. With family support and small loans, I crowdfunded my first instalment — £3,000 of the £14,000 tuition — then paid the rest throughout the year with my job as a support worker.
Now, I support five residents with different disabilities. One has dyslexia and struggles with learning, so I help him review his engineering coursework, even though my degree is in biology. Another has Down syndrome, diabetes, and other mental, psychological and health conditions, so I handle their medication and meal prep. I keep my smiling face on even when I’m having a bad day, give them their medication, and prepare their food. It was tasking at first, learning how they like their meals, but now I can whip up food that makes them happy.
The biggest adjustment for me has been learning how to provide emotional support for my residents. Back home, I never really had to consider people’s feelings. Here, I’ve had to learn patience, empathy, and how to put others first. However, I also don’t let myself get too emotionally involved; I keep my shifts strictly about work so I can focus on my personal life.
I don’t have a long-term plan yet. I just want to settle down with a partner, get my indefinite leave to remain and start a business at some point. Whatever it is, I’m staying put in the UK and grinding through the routine until I find something better.
Bottom Line
For these Nigerians, care work is more than a job. It’s a balancing act between survival and ambition. Some see it as a stepping stone, others as a struggle to stay afloat, but all of them are navigating a system that demands resilience.

Also Read: What It Really Costs to Move Out as a Young Person in Nigeria
[ad]